
Xpert® Xpress GBS
Dual target for S. agalactiae (DNA) Serotypes I-X and non-beta hemolytic in 30–42 minutes
Sign in or create a MyCepheid account to add items to cart
Test pack size(s)

10 Tests
XPRSGBS-CE-10
Qty
Unit price
Subtotal
USD
Product is not available for purchase in your region.
Collection devices
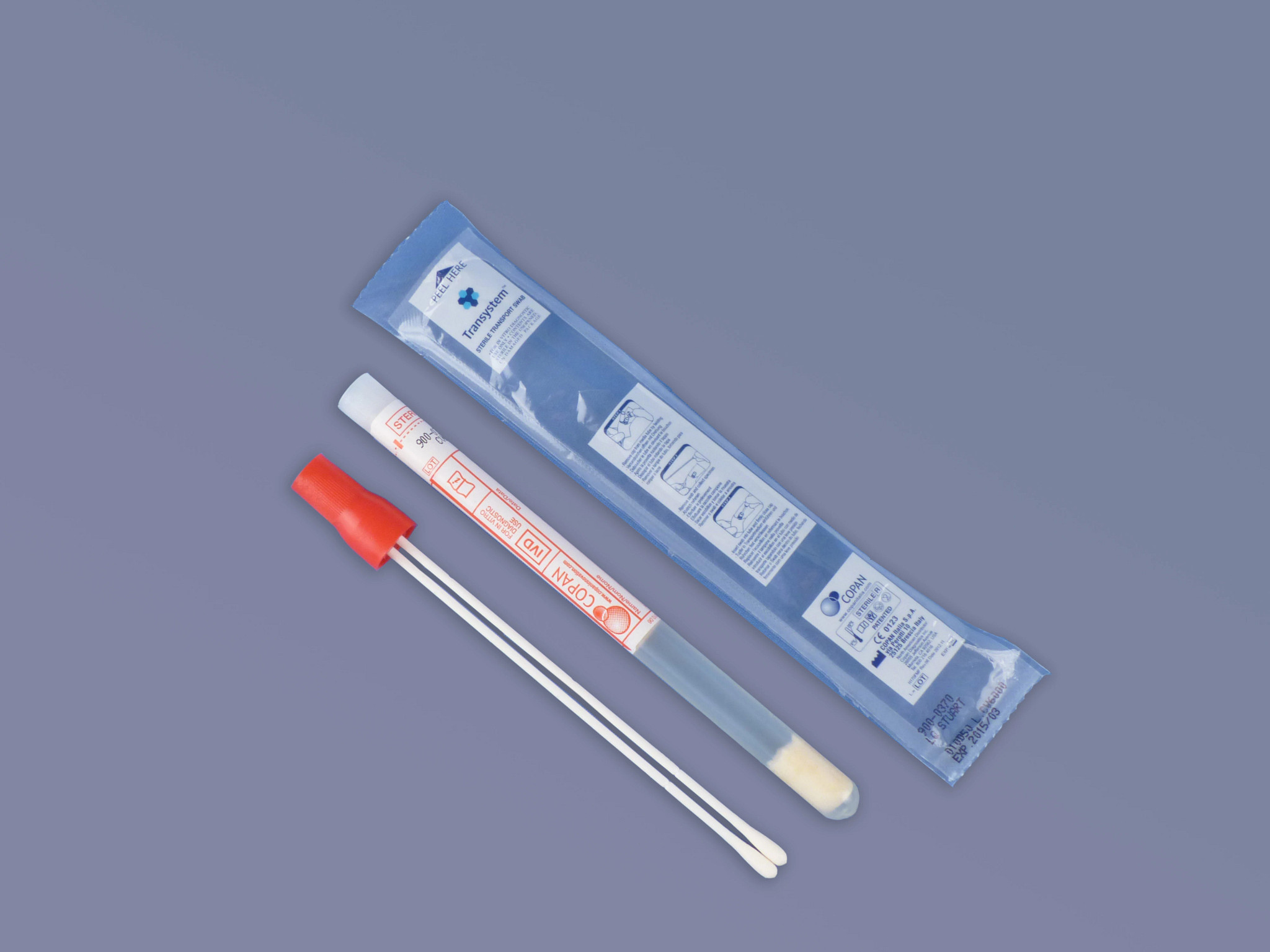
Collection Device (Pack of 50)
900-0370
Qty
Unit price
Subtotal
USD
Product is not available for purchase in your region.
Total
{{currency}}
0
Error adding items to cart. If this error persists, please contact Digital Support
The Need
Group B Streptococcus (GBS) remains a leading cause of early-onset neonatal sepsis. Rates of maternal colonization have not changed, but universal antenatal screening at 35–37 weeks along with the use of intrapartum antibiotic prophylaxis (IAP) has resulted in a decrease of early-onset disease.1
Challenges remain, including:
Challenges remain, including:
- Risk of change of GBS colonization status following screening at 35–37 weeks of gestation2,3
- Some women with unknown GBS status presenting at Labor and Delivery unit4,5
- Risk-based IAP exposes 65–85% of GBS-negative women to antibiotics6
1 Wicker E, et al. Group B streptococci: declining incidence in infants in Germany. Pediatr Infect Dis J. 2019 May;38(5):516–9.
2 Helmig R, et al. Diagnostic accuracy of polymerase chain reaction for intrapartum detection of Group B Streptococcus colonization. Acta Obstet Gynecol Scand. 2017
Sep;96(9):1070-1074.
3 Melin P. Neonatal group B streptococcal disease: from pathogenesis to preventive strategies. Clin Microbiol Infect. 2011 Sep;17(9):1294-303.
4 Di Renzo et al. Intrapartum GBS screening and antibiotic prophylaxis: a European consensus conference. J Maternal Fetal Neonatal Med. 2014:1-17. Available at: https://pubmed.
ncbi.nlm.nih.gov/25162923
5 ASM, March 2020, Guidelines for the Detection and Identification of Group B Streptococcus - Revised Guidelines from CDC, 2020
6 Saari A, et al. Antibiotic exposure in infancy and risk of being overweight in the first 24 months of life. Pediatrics. 2015 Apr;135(4):617–626.
2 Helmig R, et al. Diagnostic accuracy of polymerase chain reaction for intrapartum detection of Group B Streptococcus colonization. Acta Obstet Gynecol Scand. 2017
Sep;96(9):1070-1074.
3 Melin P. Neonatal group B streptococcal disease: from pathogenesis to preventive strategies. Clin Microbiol Infect. 2011 Sep;17(9):1294-303.
4 Di Renzo et al. Intrapartum GBS screening and antibiotic prophylaxis: a European consensus conference. J Maternal Fetal Neonatal Med. 2014:1-17. Available at: https://pubmed.
ncbi.nlm.nih.gov/25162923
5 ASM, March 2020, Guidelines for the Detection and Identification of Group B Streptococcus - Revised Guidelines from CDC, 2020
6 Saari A, et al. Antibiotic exposure in infancy and risk of being overweight in the first 24 months of life. Pediatrics. 2015 Apr;135(4):617–626.
The Solution
- The Xpert Xpress GBS test is a qualitative in vitro diagnostic test intended for the detection of DNA from Group B Streptococcus (GBS). The test is performed using a dual vaginal/rectal swab specimen collected from pregnant females during antepartum or intrapartum.
- The Xpert Xpress GBS test is intended to aid in the diagnosis of GBS colonization to identify candidates for antibiotic prophylaxis.
The Impact
- Identify GBS colonization status at the right time, at the time of labor (intrapartum).4
- Identifying more women with GBS at the time of delivery and providing them with timely Intrapartum Antibiotic Prophylaxis (IAP) may result in an reduction of early-onset GBS disease in neonates.7
- Fast and easy-to-interpret results enable adequate IAP delivered to mothers with unknown status, which may result in less impact on the newborn intestinal flora.8,9
7 El Helali et al. Diagnostic Accuracy of a Rapid Real-Time Polymerase Chain Reaction Assay for Universal Intrapartum Group B Streptococcus Screening. Clin Infect Dis. (2009) 49 (3):
417-423.
8 Björklund V, et al. Replacing risk-based early-onset-disease prevention with intrapartum group B streptococcus PCR testing. J Matern Fetal Neonatal Med. 2017 Feb;30(3):368-373
9 Zimmermann P, et al. Effect of intrapartum antibiotics on the intestinal microbiota of infants: a systematic review. Arch Dis Child Fetal Neonatal Ed. 2020 Mar;105(2):201–8
CE 2797
417-423.
8 Björklund V, et al. Replacing risk-based early-onset-disease prevention with intrapartum group B streptococcus PCR testing. J Matern Fetal Neonatal Med. 2017 Feb;30(3):368-373
9 Zimmermann P, et al. Effect of intrapartum antibiotics on the intestinal microbiota of infants: a systematic review. Arch Dis Child Fetal Neonatal Ed. 2020 Mar;105(2):201–8
CE 2797







